Cancer research has long been one of the most complex and challenging areas of medical science. However, in recent years, there have been significant breakthroughs that are offering new hope for patients and medical professionals alike. With advancements in immunotherapy, precision medicine, and gene editing, researchers are uncovering innovative treatments that may ultimately transform the way we approach cancer.
In this post, we’ll explore some of the most promising discoveries in cancer treatment, their potential to improve outcomes, and how they could reshape the future of oncology.
1. Immunotherapy: Harnessing the Power of the Immune System
Immunotherapy, a treatment that uses the body’s own immune system to fight cancer, has emerged as one of the most revolutionary approaches in recent cancer research. Unlike traditional treatments like chemotherapy, which target both healthy and cancerous cells, immunotherapy is designed to specifically target cancer cells, minimizing damage to surrounding tissue.
Checkpoint Inhibitors
One of the most significant breakthroughs in immunotherapy has been the development of checkpoint inhibitors. These drugs work by blocking certain proteins, called checkpoints, that prevent immune cells from attacking cancer cells. By inhibiting these checkpoints, such as PD-1 and CTLA-4, the immune system can better recognize and destroy cancer cells.
Drugs like Keytruda (pembrolizumab) and Opdivo (nivolumab) have shown remarkable success in treating cancers like melanoma, lung cancer, and non-Hodgkin lymphoma. In some cases, patients who had no other treatment options available have experienced long-term remission or even complete recovery.
CAR-T Cell Therapy
Another cutting-edge approach within immunotherapy is CAR-T cell therapy (Chimeric Antigen Receptor T-cell therapy). This process involves modifying a patient’s own T cells in the lab to better recognize and attack cancer cells. CAR-T therapies have shown tremendous promise in treating blood cancers like leukemia and lymphoma, with some patients experiencing remarkable, life-saving results.
Recently, CAR-T therapies have expanded into solid tumors, which have historically been more challenging to treat. While still in the experimental phase for certain cancers, ongoing research into improving CAR-T therapy could dramatically increase its effectiveness and reduce side effects, making it a powerful tool in cancer treatment.
2. Precision Medicine: Tailoring Treatment to the Individual
Precision medicine, also known as personalized medicine, is another major breakthrough in cancer research. This approach involves tailoring treatment plans based on the unique genetic makeup of a patient’s cancer. Rather than applying a one-size-fits-all treatment, precision medicine seeks to identify the specific mutations and characteristics of a tumor, and then select therapies that target those abnormalities.
Genomic Profiling and Targeted Therapy
Advancements in genomic profiling have made it possible to sequence the DNA of tumors and identify specific genetic mutations driving cancer growth. By understanding these mutations, doctors can use targeted therapies that attack only the cancerous cells while sparing healthy cells.
For example, the drug Herceptin (trastuzumab) is used to treat breast cancer patients whose tumors overexpress the HER2 protein, a genetic mutation that promotes tumor growth. Similarly, targeted therapies like Gleevec (imatinib) have been groundbreaking for chronic myelogenous leukemia (CML), targeting the specific BCR-ABL fusion gene that causes the disease.
As genetic testing becomes more affordable and accessible, precision medicine is expected to become an even more integral part of cancer treatment, with more therapies tailored to the specific needs of patients.
3. Gene Editing: A Revolutionary Tool for Cancer Treatment
Gene editing, particularly through CRISPR-Cas9 technology, is a breakthrough that could revolutionize the way we treat cancer. This technology allows scientists to precisely modify DNA within cells, potentially correcting genetic mutations that cause cancer or even reprogramming immune cells to better target cancer cells.
CRISPR-Cas9 and Cancer Research
CRISPR-Cas9 is a tool that acts like “genetic scissors,” cutting out faulty genes and replacing them with healthy ones. While still in its early stages, CRISPR technology has shown potential in cancer research by targeting genes that contribute to cancer progression. Researchers are exploring how CRISPR can be used to modify immune cells, remove cancer-promoting mutations, or enhance the body’s natural defenses against tumors.
In clinical trials, CRISPR has been used to edit immune cells to improve their ability to recognize and destroy cancer cells. Although the technology is still experimental, its success in early studies suggests that gene editing could play a pivotal role in developing new, highly effective cancer therapies.
Gene Therapy for Cancer Treatment
Gene therapy, which involves introducing or altering genetic material within a patient’s cells to treat or prevent disease, is also showing promise in oncology. One approach involves inserting genes into a patient’s immune cells to enhance their ability to recognize and fight cancer. Clinical trials using gene therapy to treat cancers like melanoma, lung cancer, and prostate cancer have demonstrated positive results, though further studies are needed to fully assess their safety and efficacy.
4. Liquid Biopsy: A Non-Invasive Diagnostic Tool
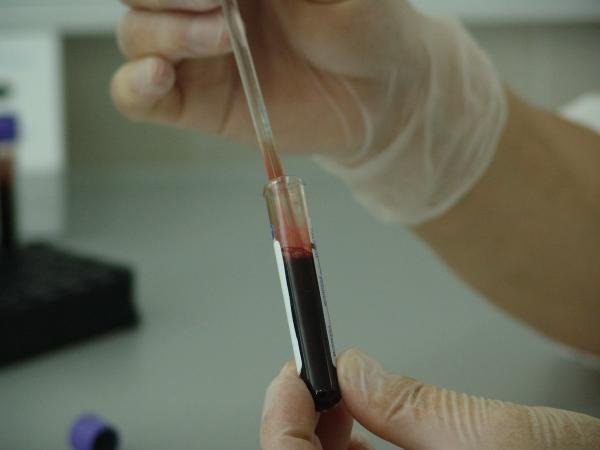
In the past, diagnosing and monitoring cancer often required invasive procedures like biopsies. However, a liquid biopsy is a groundbreaking non-invasive alternative that detects cancer-related genetic material from a simple blood test.
How Liquid Biopsy Works
Liquid biopsy detects circulating tumor DNA (ctDNA) or circulating tumor cells (CTCs) in the blood. This allows doctors to identify the presence of cancer, monitor its progression, and even assess how well a patient is responding to treatment—all without the need for a traditional biopsy.
One of the key advantages of liquid biopsy is that it can detect cancer at earlier stages and is especially useful for tracking cancer in patients who may not be suitable candidates for traditional biopsy. Additionally, liquid biopsies have been used to detect minimal residual disease—microscopic amounts of cancer cells left behind after treatment that can lead to relapse.
Early Detection and Monitoring
Liquid biopsy has the potential to change the way cancer is diagnosed and monitored. Early detection of cancers, especially those that are difficult to screen for (such as pancreatic cancer or ovarian cancer), could greatly improve survival rates. Additionally, it can help in identifying new mutations that may allow clinicians to switch to more effective treatments, improving patient outcomes.
5. Artificial Intelligence and Machine Learning in Cancer Research
AI and machine learning (ML) are increasingly playing a role in cancer research and treatment. These technologies are being used to analyze large datasets, identify patterns in cancer progression, and assist in drug development.
AI in Drug Discovery
AI can help researchers sift through vast amounts of data to identify potential drug candidates. For example, AI models can predict how different compounds might interact with specific cancer cell types, speeding up the process of drug discovery. In recent years, AI has been used to help identify new cancer treatments, including therapies that target previously “undruggable” cancer mutations.
AI for Early Detection
AI is also improving cancer detection. Deep learning algorithms are being used to analyze medical imaging (e.g., X-rays, MRIs, and CT scans) with remarkable accuracy, detecting abnormalities that may be missed by human doctors. Early detection using AI can lead to quicker diagnoses, more accurate staging of cancer, and more effective treatment plans.
AI in Precision Oncology
AI is enabling a more precise approach to oncology by analyzing genetic data and patient records to develop personalized treatment plans. In combination with genomic profiling, AI can help predict how a patient’s cancer will respond to specific therapies, offering more targeted and effective treatment options.
6. Cancer Vaccines: Preventing Cancer Before It Starts
Vaccines have long been used to prevent infectious diseases, but researchers are now working on cancer vaccines that could help prevent certain types of cancer or treat cancer once it has developed.
Preventive Vaccines
Some vaccines, like the HPV vaccine (human papillomavirus), have already been proven to prevent cancers caused by viruses. The HPV vaccine has been shown to reduce the risk of cervical cancer and other cancers caused by HPV, such as anal, throat, and penile cancers. There are also vaccines in development aimed at preventing liver cancer (by targeting the hepatitis B virus) and other virus-related cancers.
Therapeutic Cancer Vaccines
Therapeutic vaccines are designed to treat existing cancers by stimulating the immune system to recognize and destroy cancer cells. These vaccines aim to “train” the immune system to identify specific proteins or mutations present on cancer cells, triggering an immune response. Trials for vaccines targeting cancers like melanoma, prostate cancer, and non-small cell lung cancer are ongoing, and while results have been mixed, some patients have experienced significant improvements.
The Future of Cancer Treatment: A Hopeful Horizon
The breakthroughs in cancer research are providing new hope to patients and doctors alike. While challenges remain, the future of cancer treatment looks incredibly promising. With more targeted therapies, personalized treatments, and new technologies like AI and gene editing, researchers are moving closer to the goal of curing cancer or managing it as a chronic disease.
As these treatments progress through clinical trials and become more widely available, cancer may no longer be seen as a terminal diagnosis, but as a treatable and manageable condition. Though there is still much to be done, the landscape of oncology is transforming in ways that were unimaginable just a few decades ago, offering hope to millions of people affected by cancer worldwide.